The antiquity of human malaria has been recorded in the Ebers Papyrus (ca. 1570 B.C.), in clay tablets from the library at Ashurbanipal (2000 B.C) and in the classic Chinese medical text the Nei Ching (2700B.C). These describe the enlarged spleen, periodic fevers, as well as headache, chills and fever. Malaria probably came to Europe from Africa via the Nile Valley or it was the result of closer contact between Europeans and the people of Asia Minor. The Greek physician Hippocrates (460-370B.C.) discussed in his “Book of Epidemics” the two kinds of malaria, one with recurrent fevers every third day (benign tertian) and another with fevers on the fourth day (quartan). He also noted that those living near marshes had enlarged spleens. Hippocrates did not describe malignant tertian malaria but by 200B.C. there is clear evidence of this malaria being present in the Roman Republic. Indeed, the disease was so prevalent in the marshland of the Roman Campagna that the condition was called the Roman Fever. Since it was believed that this recurrent fever occurring during the sickly summer season was due to vapors emanating from the marshes it was called by the Italian name mal’ aria literally bad air. Over the centuries malaria spread across; by the 14th century it was in England. Malaria was brought to the New World by European explorers, conquistadors, colonists and African slaves, and by the 1800’s it was worldwide in geographic distribution.
Victims of malaria characteristically had enlarged and blackened spleens and livers due to the presence of a particulate blackish-brown pigment. Heinrich Meckel (in 1847) proposed that this pigment, called hemozoin, was the cause of malaria. However, though Meckel was incorrect, malaria pigment became critical to the discovery of the parasite and its vector.
Charles Louis Alphonse Laveran (1845-1922), a physician in the French Foreign Legion in Algeria on October 20, 1880, examined under the microscope a drop of blood taken from a soldier suffering with malaria fever. He found within the red cells transparent globules containing hemozoin, and on occasion he found mobile filaments emerging from the clear spherical bodies (called exflagellation).
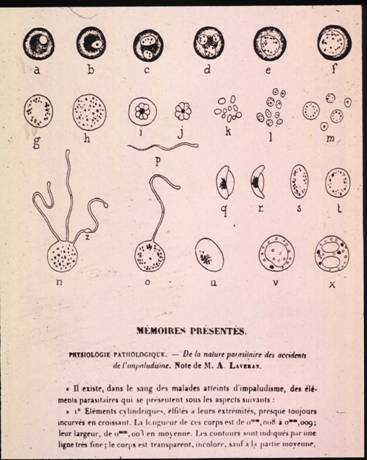
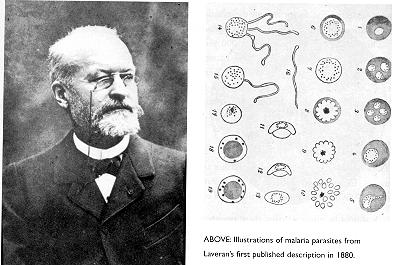
Laveran’s drawings of malaria parasites in the blood
He also found that some malaria patients had crescents. In effect, Laveran had discovered an animal parasite with different developmental stages. Initially his work was received with skepticism but by 1884 the Italian workers E. Marchiafava, A. Celli and C. Tomassi-Crudeli had confirmed his findings and 6 years later Camillo Golgi (1843-1926) described asexual multiplication ( merogony or schizogony). In 1891 Dimitri Romanowsky (1861-1921) developed a staining technique that enabled workers using better microscopes and oil immersion lenses to clearly distinguish the nucleus and cytoplasm of the parasite.
The significance of Laveran’s observation of exflagellation went unappreciated until 1896-97 when William MacCallum and Eugene Opie, students at Johns Hopkins University, found that the blood sparrows and crows infected with Hemoproteus (a bird parasite closely related to malaria) contained two kinds of sex cells, the gametocytes, and exflagellation represented the release of microgametes from the male gametocyte. They also correctly interpreted their observations: gametocytes occur in the blood and when ingested by a mosquito, the gametes are released in the mosquito stomach, where fertilization takes place and this results in a wormlike zygote, the ookinete.
However, there remained a mystery: How did one acquire malaria? In 1898 Ronald Ross (1857-1932) a Surgeon-Major in the British Indian Medical Service described the development of the malaria parasite in the mosquito.
|
|
|
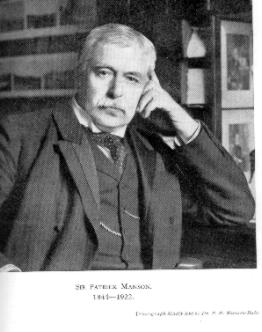
Patrick Manson (1844-1922), who discovered that the worms of elephantiasis could be transmitted by mosquitoes, encouraged Ross to study mosquito transmission and he suggested that this might be accomplished by trailing the parasite through its telltale pigment hemozoin. Working with bird malaria Ross described that 4 days after ingestion of crescents (gametocytes) large bodies containing hemozoin appeared on the mosquito stomach; over the next several days these bodies grew in size.


Ross’ drawings of oocysts on mosquito stomach (4), and sporozoites in salivary gland (5)
A Historical Digression
Ross had discovered the stage after the ookinete, the oocyst. In the summer of 1898 Ross found that the parasites, which had developed in the oocysts, the sporozoites, were liberated and then migrated to the mosquito salivary glands. Although Ross did not describe the development of the human malaria parasite in the mosquito, credit for that goes to the Italians especially Giovanni Batistta Grassi, Amico Bignami, Giovanni Bastianelli, Angelo Celli and Antonio Dionisi, he had clearly flagged the mosquito as this disease’s vector. Ross communicated his findings on July 28, 1898 and left India for England in February 1899. Manson was convinced by Ronald Ross that mosquitoes could possibly transmit malaria. To test this theory he actually allowed Anopheles mosquitoes which had fed on a tertian malaria patient to bite his own son and his son came down with malaria! He then went with some friends to the Roman Compagna near Ostia, which was notorious for malaria, and lived in a mosquito-proof hut from July to October; he and his friends remained in perfect health, although, I imagine, somewhat bored. These experiments established clearly that mosquitoes carried malaria.
Within months after Ross’ communication the Italians described the development of 3 species of human malarias in the anopheline mosquito and were able to transmit malaria to a healthy volunteer by the bite of an infected mosquito. It was, as Ross had correctly surmised, similar to that of the bird malaria with which he had worked. It is the breeding sites of mosquitoes that explain the association of the disease with swampy, marshy areas of the world.
Although malaria can be induced by the introduction of sporozoites through the bite of an infectious female mosquito the parasites do not appear immediately in the blood. This was surprising in view of the fact that in 1903 Fritz Schaudinn claimed to have seen sporozoites directly invade erythrocytes. Schaudinn was a dominant figure in parasitology so few doubted his word, but over time since no one could repeat his observations it was called into question. First in birds and then in primates it was shown that a tissue (or exo-erythrocytic) phase developed after inoculation of sporozoites, and only later did parasites appear within erythrocytes. In 1948 HE Shortt, PCC Garnham and their colleagues found exo-erythrocytic stages in the livers of rhesus monkeys infected with P. cynomolgi (a parasite similar to the benign tertian malaria, P. vivax of humans) and later they demonstrated similar stages in biopsy material taken from the livers of human volunteers infected by the bite of mosquitoes carrying P. vivax. Subsequently, this stage at the same site was described for the malignant tertian malaria, P. falciparum.
A lecture by Dr. Irwin Sherman - Impersonation of Ronald Ross
Ronald Ross (1857 - 1932)
(Ross, age 60, has completed his memoirs, which he carries with him. He enters the room. He has piercing eyes, is balding, gray at the temples and with a gray handlebar mustache. He wears his trademark bow tie.)
William Shakespeare, in his play the tempest, had one of his characters, Caliban, curse the master who had enslaved him, saying
"All the infections that the sun sucks up from bogs, fens, flats on prosper fall and make him by inch-meal a disease."
The curse was a deadly fever recognized by many in Shakespeare's England in the 1600's, but one that was more prevalent in the tropics. The fever is, of course, malaria -- a disease that has plagued humankind since the earliest of times. The great physician of ancient Greece, Hippocrates, recognized and described very accurately the intermittent chills and fever of malaria more than 2,000 years ago. And, he also observed the association of malaria with bogs, marshes and swamps, but he did not understand the connection.
Although malaria was known since earliest recorded history, the cause of the disease was only discovered in 1880. The man who found this killer-parasite was Alphonse Laveran, a medical officer in the French army stationed in Algeria who, when he examined a drop of blood taken from a soldier ill with malaria with his crude microscope, found crescents and spheres that were specked with a blackish brown pigment. Observing this blood, he saw filaments emerging from the crescent; these moved back and forth like whips. No, I am not Laveran, I am surgeon-major Ronald Ross, Knight Commander of Bath, Knight Commander of the Order of St. Michael and St. George, presently professor at the Liverpool School of Tropical Medicine, and recipient of the 1902 Nobel Prize for my work on malaria about which I will speak shortly.
Malaria, as most of us know it today (thanks to Monsier Laveran), is a disease of the blood. The chills and fever are due to parasites multiplying in our red blood cells; these they destroy, causing anemia and, in some cases, the result is death. Even when death does not occur, the disease is still debilitating; individuals cannot work and must remain in bed. Consequently, malaria saps the vigor of the patient and the economy of the country suffers. There are, this very day, more than 2 billion people at risk and more than 200 million cases of malaria. And, each year, there are more than 2 million deaths -- mostly in African children. So, you see, identifying the parasite as did Laveran more than 100 years ago does not ipso facto produce eradication of the disease. Malaria is a disease of both the past and the present. Indeed, you will be as shocked as I am to know that, although malaria has been eliminated from many parts of the world (such as the United States, Europe, Great Britain, Japan, the countries that comprise the former Soviet Union and Australia), it remains prevalent in 102 countries (mostly in Africa, S.E. Asia and South America) and there are more cases of malaria today than ever before. I will return to this point -- why we have so much malaria today -- later.
I am British, but was born on Friday, May 13, 1857, in India. I am the eldest Ross child. My father was an officer in the British Army stationed in India which, at that time, was a part of the British Empire. It was in India that I first experienced malaria -- my father had it and we had to take quinine with regularity to ward off the fever. Sometimes, it worked; many times, it did not. As a boy of 8, I was sent by my parents to England to be educated. I was a dreamer and, although I liked mathematics, I preferred wandering around the countryside, observing and collecting plants and animals. At Springhill Boarding School, which I attended from the age of 12, I began to write poetry, painted watercolors and thought of becoming an artist. But, my father had other ideas -- study medicine in London, he said. So, at age 17 (following his orders), I began medical studies in preparation (as my father had suggested) for entry into the Indian Medical Service. I was not a good student, not because I was lazy, but because I had so many other interests I could not concentrate on medicine. I did pass my examinations (after failing them the first time) and then worked as a ship's doctor and later entered the Indian Medical Service. I was posted to Bombay, Madras and Bangalore. At most of these posts, life was a dull routine --a couple of hours of work each morning examining the ill and an occasional evening of duty. The rest of the time was free to write poetry, to play my violin, to paint and to study languages. Much of my writing was unappreciated; publishers rejected the poems and novels, so I published them at my own expense.
On my first leave home, I met and married my wife Rosa.
I returned to England on a second leave in 1894 and, by that time, had spent 13 years in India. My scientific accomplishments were few: I wrote a few papers on malaria in the Indian Medical Gazette; failed to confirm Laveran's findings of malaria parasites in the blood; and even claimed that malaria was primarily an intestinal infection. What a fool I! Everything I had tried had failed.
A perplexing and unsolved question regarding malaria was: how does one become infected with malaria?
Then, in 1894 (April 9th, to be exact), I visited with Dr. Patrick Manson. It was Manson who, while working in China, had shown that mosquitoes carry filaria -- the worms that cause the disease elephantiasis. Dr. Manson was an outstanding microscopist and he showed me Laveran's parasite peppered with a black/brown pigment. He also provided me with the accumulating literature on malaria parasites; he became my mentor. One day, as we were walking along Oxford Street, Manson said to me, "I have formed the theory that mosquitoes carry malaria. The mosquitoes suck the blood of people sick with malaria -- the blood has the parasites described by Laveran -- they get into the mosquito stomach, shoot out those whips -- and the whips get into the mosquito body, where they turn into a spore like those of anthrax. . . . The mosquito dies, falls into water and, when people drink a soup of dead mosquitoes, they get malaria."
This was not as farfetched as it might sound, although Dr. Manson did not have a shred of evidence for his mosquito theory. As I mentioned earlier, the association of malaria with swamps and marshes was known for thousands of years; indeed, the association was so strong that the disease takes its name -- bad air or malair/ia -- from the vapors emanating from the damp, low lying land. And, before Laveran's discovery of the protozoan parasite that causes malaria, two of Koch's associates claimed to have isolated from the air and mud of malarious marshes and also from the urine of a patient with malaria a rod-like bacterium which they called bacillus malaria. But, since no one could ever cultivate this bacterium, it was forgotten, and that was to the good.
I left England in March, 1895, and reached Bombay a month later. I had a mission: find the means of malaria transmission.
In June, 1895, encouraged by Manson, I set up an experiment by allowing the water in which the infected mosquito had laid her eggs and in which her progeny had been swimming, to die. The water was then given to a volunteer to drink. The man came down with a fever but, after a few days, I could find no crescents in his blood. The same experiment was repeated with two other men who were paid for their services. Failure again. So, it appeared that drinking water with mosquito-infected material did not produce the disease. I began to think that, perhaps, the mosquitoes had the disease, but that they probably gave it to human beings by biting them and not by being eaten in the form of spores. (He writes on the board the words "INOCULATION" "INGESTION".) Inoculation, not ingestion, was probably the mode of transmission. (He puts a line through the word "INGESTION".)
Being an army man in the Indian Medical Service had many disadvantages and, frequently, I was sent on very short notice to different posts. My malaria work was interrupted by my being dispatched to Bangalore to try to stop a cholera epidemic, which I did by prescribing a new system of drains. After the cholera situation in Bangalore resolved itself, I set out, once again, on the mosquito-malaria trail.
At this point, I must tell you a bit about what we knew concerning the development of the malaria parasite in the blood when I began my search. The malaria parasite penetrates the red cell, begins to digest hemoglobin and produces a black/brown speckled pigment; these parasites produce many offspring which can repeat the cycle again and again. The release of these offspring and destruction of the red cell coincides with the fevers and chills. There are other parasites that do not divide upon entering a red blood cell -- instead, these develop into crescents and these stages give rise to the whips, which we believed (incorrectly, I must admit) to be flagella. The crescents are, in fact, the gametes or sex cells, with the whiplike bodies being analogous to sperm, that is, they are the male gametes.
(Here, he shows a slide of the development of malaria in the blood.)
Immediately, I began work with patients whose blood contained crescent-shaped malaria parasites, and with mosquitoes bred from larvae. My first task was to get the mosquitoes to bite the patients. It was like looking for a needle in a haystack. There are more than 2500 different kinds of mosquitoes and, at the time, there were no good means for identifying most of them. I worked mostly with the gray and brindled kind. Although, when I dissected the mosquitoes, I found that there were the whiplike extensions in the mosquito stomach (he draws on board) -- we call this exflagellation -- there was no further development. This result was no more informative than what laveran had seen in a drop of blood on a microscope slide nearly 20 years earlier. I failed time and time again.
Today, I understand (as I did not then) why this was so: the gray mosquitoes are Culex and the brindled ones are Aedes and these do not carry human malaria. No, the one I really should have used was the brown, dapple-winged mosquito, the Anopheles, but I did not recognize this for the entire year I dissected mosquitoes. Thousands of mosquito carcasses was all I had to show for my labors and each mosquito dissection required hours of my effort at the microscope. I wrote to Manson of my lack of success and he very kindly, as always, responded with words of encouragement.
Then, in August, 1897 -- I was now 40 years old and had spent 17 years in the Indian Medical Service -- I turned from the incompetent species of mosquito to the competent, brown, dapple-winged Anopheles. On August 16, 1897, my assistant brought me one of the bottles in which mosquitoes were being hatched from larvae. It contained as I have written in my memoirs (and here opens the book to read) "about a dozen big brown fellows, with fine tapered bodies and spotted wings (i.e., Anopheles) hungrily trying to escape through the gauze covering of the flask which the angel of fate had given my humble retainer! There are about 50 different species of Anopheles. They bite at night, have spotted wings and sit on a wall with the tail sloping away from it. Their eggs are boat-shaped, laid singly and often tied together, touching each other, end to end. The larvae have no breathing tube, but float flat on the surface of the water like sticks. Each of the mosquitoes was given a number and as usual I decided that I would record in my notebook, with drawings, what I found in each mosquito.
My mind was blank with the August heat; the screws of the microscope were rusted with sweat from my forehead and hands, while the last remaining eyepiece was cracked. I fed them on Husein Khan, a patient who had crescents in his blood.
There had been some casualties among the mosquitoes, and only three of the Anopheles were left on the morning of August 20, 1897. One of these had died and swelled up with decay. At 7 a.m., I went to the hospital, examined patients, attended to correspondence and dissected the dead mosquito, without result. Then -- a significant reminder of one of those unknown quantities in the equation to be solved -- I examined an Anopheles. No result again. At about 1 p.m., I determined to sacrifice the last Anopheles. Was it worth bothering about the last one, I asked myself. And, I answered myself, better finish off the batch. A job worth doing at all is worth doing well.
The dissection was excellent and I went carefully through the tissues, now so familiar to me, searching every micron with the same passion and care as one would have in searching some vast ruined palace for a little hidden treasure. Nothing. No; these new mosquitoes also were going to be a failure: there was something wrong with the theory. But the stomach tissues still remained to be examined -- lying there, empty and flaccid, before me on the glass slide, a great white expanse of cells like a large courtyard of flagstones, each one of which must be scrutinized -- half an hour's labor at least. I was tired and what was the use? I must have examined the stomachs of a thousand mosquitoes by this time. But the angel of fate fortunately laid his hand on my head, and I had scarcely commenced the search again when I saw a clear and almost perfectly circular outline before me of about 12 microns in diameter. The outline was too sharp, the cell too small to be an ordinary stomach cell of a mosquito. I looked a little further. Here was another, and another exactly similar cell.
The afternoon was very hot and overcast; and I remember opening the diaphragm of the substage condenser of the microscope to admit more light and then changing the focus. In each of these, there was a cluster of small granules, black as jet, and exactly like the black pigment granules of the Plasmodium crescents. I made little pen-and-ink drawings of the cells with black dots in them. The next day, I wrote the following verses and sent these to my dear wife:
This
day relenting God
Hath placed within my hand
A wondrous thing; and God
be praised. At his command,
Seeking his secret deeds
With tears and toiling breath,
I find thy cunning seeds,
O million-murdering death.
I know this little thing
A myriad men will save.
O death, where is thy sting?
Thy victory, O grave?
Here was the clue. I had shown that, four or five days after feeding on infected blood, the mosquito had oocysts on its stomach. But, did these keep on growing, and how did these mosquitoes become infective? I planned to answer these questions shortly but, before that work could begin, I reported my findings to the British Medical Journal in a paper entitled, "On some peculiar pigmented cells found in two mosquitoes fed on malarial blood." It appeared December 18, 1897.
I knew I could wrap up the unfinished work in a matter of a few weeks, but then I was struck by a blow from the Indian Medical Service. I was ordered to proceed to Calcutta -- immediately.
As soon as I arrived in Calcutta, I set my hospital assistants the task of hunting for mosquito larvae and pupae. I soon got a stock of the dapple-winged mosquitoes, and set about getting them to bite patients who were suffering from malaria. I flooded some ground outside the laboratory, in the hope to imitate rain puddles and see if we could learn something about mosquito breeding.
"If I am not on the pigmented cells again in a week or two," I wrote to Manson, "my language will be dreadful."
In Calcutta, I was given a laboratory which consisted of two sizable rooms, offices and a cool and shady veranda. There were two Indian assistants who had already been working there when I arrived, but they were old men and not very intelligent. I engaged two younger men, Purboona and Mahomed Bux. Both of these, I paid out of my pocket. I engaged Mahomed Bux because he looked the most rascally of all those who came to apply for work and I thought that such a scoundrel must be intelligent.
However, there were not a large number of malaria cases in the Calcutta hospitals. So, I turned to something which I had thought about previously -- the study of mosquitoes and malaria, as seen in birds. I caught pigeons, crows, larks and sparrows, setting out cages on two old hospital beds. Mosquito nets were put over the beds and then, at night, infected mosquitoes were put under the nets. Before much time had passed, I found that crows and pigeons had some of the malaria parasites in their blood; also, I found the pigmented cells, which I had first spotted in the stomachs of mosquitoes which had been fed on infected larks.
I wrote to Manson almost every day; I was sure of the whole life-history of the mosquito, except I had not actually seen the zygotes, those spherical cells into which the flagella had penetrated, turning into oocysts. This was the last stage in the study. I found that the cells depended, as regards their size, exactly on the length of time since the mosquitoes had been fed on infected blood. The parasites grew to their maximum size about six days after the feed of infected blood had been given. They left the stomach after this time; but what happened to them then? This was the next task I had to carry out.
Then, one day, I was studying some sparrows. One was quite healthy, another contained a few of the malaria parasites, the third had a large number. Each bird was put under a separate mosquito net and exposed to a group of mosquitoes from a batch that had been hatched out from grubs in the same bottle. Fifteen mosquitoes were fed on the healthy sparrow; in their stomachs, not one parasite was found. Nineteen mosquitoes were fed on the second sparrow; every one of these contained some parasites, though, in some cases, not very many. Twenty insects were fed on the third, badly infected, sparrow; every one of these contained some parasites in their stomachs and some contained huge numbers.
This delighted me and I wrote to Manson that it was a beautiful piece of work. I asked the medical service for assistance and a leave, but was denied this.
Manson wrote an article in the British Medical Journal describing the work I had done; the British Medical Association Conference was to meet in Edinburgh in July, with a special new section devoted to the study of tropical diseases, with Manson as its president. I wanted to provide the final story of the malaria parasite for this meeting; but, I knew that time was very short. I still did not have the full details of sporulation -- that is, the change from the oocysts in the mosquito's stomach into the stages that could infect human beings and birds.
Then, I found that some of the oocysts seemed to have stripes or ridges in them; this happened on the 7th or 8th day after the mosquito had been fed on infected blood. I spent hours every day peering into the microscope and wrote to Manson: "The constant strain on mind and eye at this temperature is making me thoroughly ill."
I thought no doubt these oocysts with the stripes or rods burst -- but then what happened to them? When they burst, did they produce the same stages that infected human blood?
Then, on July 4, 1898, I got something of value. Near a mosquito's head, I found a large branch-looking gland. It led into the head of the mosquito. I said to myself, "It is a thousand to one that it is a salivary gland." Did this gland infect healthy creatures? Did it mean that if an infected mosquito fed off the blood of an uninfected human being or bird, then this gland would pour some of the parasites, now in the form of sporozoites, into the blood of the healthy creature?
During July 21 and 22 of that year, I took some uninfected sparrows, allowed mosquitoes (which had been fed on malarious sparrows) to bite them and then, within a few days, was able to show that the healthy sparrows had become infected. This was the proof -- this showed that malaria was not conveyed by dust or bad air. After all, men and birds don't go about eating dead mosquitoes.
On July 25, now sure, I sent off a triumphant telegram to Sir Patrick Manson, reporting the complete solution; three days later, Manson spoke at the British Medical Association meeting in Edinburgh, describing the long and painstaking piece of research which I had been carrying out for years past.
On the morning of August 13, Mahomed Bux and I released all our poor little feathered prisoners. May their little souls be living forever among eternal flowers and berries in some avian heaven.
Some of you may now sneer at this discovery, but consider this: Why would you have chosen the mosquito as the transmitter in the first place? Which kind of mosquito out of 2,500 different species would you have chosen as the transmitter? Then, how long would you expect it to take for the mosquito to become infective after it has bitten an infected individual? What part of the mosquito body would you look at to find the parasite? Let me make a comparison: examining the stomach of a mosquito under the microscope for the malaria parasite stage -- we call it an oocyst -- is comparable to searching for something the size of a ping pong ball in a body as large as a rhinoceros. So, it took persistence, perspiration and perspicacity to find the transmitter of Plasmodium -- that is the scientific name of the malaria parasite.
And now, unfortunately, I must digress to speak about the Italians, Battista Grassi, Amico Bignami and Giovani Bastianelli. Some have referred to my disagreement with them as the Roman Quarrel. The word quarrel does not begin to describe these cheats and liars who tried to steal the glory of the discovery of the mosquito transmission of malaria for themselves. As I said earlier, malaria was known in ancient Greece, and this was also true within the Roman Empire. It was particularly abundant in the low, marshy areas around Rome -- and that's the reason for the use of the Italian-derived word for the disease -- malaria.
After reading of my work on the transmission of malaria using birds, Grassi and his colleagues recognized that there were two main tasks left: to identify the mosquito that transmitted human malaria, and to demonstrate the mosquito cycle for human malaria. The Italians had many malaria patients on whom they could work, and they had lots of zanzaroni -- Anopheles. Grassi recognized that only in those areas where there was Anopheles was there human malaria, and that Culex was not involved, but he did not publish this or the development of the parasite in these mosquitoes in collaboration with Bignami and Bastianelli, until 1898. They exactly duplicated my work, but they scarcely mentioned my discovery, though they had followed my procedures step by step. It was piracy, if not plagiarism. And, that arrogant bastard Grassi never apologized, though later his two colleagues did. It is true I did not complete the proof of mosquito transmission with human malaria; the Italians did that. But, it was I who flagged the dapple-winged mosquito as the transmitter and Grassi's contribution was to simply recognize this as Anopheles. So, Grassi and I were not, as he would like you to believe, co-discoverers. I was the explorer at the helm of the ship and the Italians simply rode the decks and helped make a landing. It is fitting, therefore, that the Nobel Prize was given to me alone.
Thus we have, so to speak, closed the loop. The transmission of malaria involves development in the blood and development in the mosquito. The mosquito gets infected by biting an infected human and, in the stomach, the male and female gametes fertilize. The resulting fertilized female gamete -- or zygote -- migrates through the stomach wall and encysts there still carrying its telltale speckles of pigment. This is the oocyst. In the oocyst are formed thousands of sporozoites and, when the oocyst bursts, the sporozoites are released and these eventually find their way to the mosquito's salivary gland. This development of the parasite from stomach to salivary gland takes about a week. When such a female mosquito sucks blood, the sporozoites are injected with the saliva and the person becomes infected.
(Here, he shows a slide of the life cycle.)
One further mystery was: since sporozoites do not directly infect red cells, where do the sporozoites go before the blood becomes infected with crescents and pigmented globules? The discovery that sporozoites penetrate the liver cells and first multiply here, and that it is the parasite progeny from the liver that go on to infect red cells, was made only in the 1940's. So, there really are three cycles: one in the liver; one in the red blood cells; and one in the mosquito.
(He shows a slide with the three cycles.)
My discovery of the mosquito as a transmitter of malaria opened up new prospects for conquering not only this disease, but other diseases that were carried by this insect. I have devoted the rest of my professional life to the eradication of disease by sanitation. In some cases, by destroying the breeding sites of the mosquitoes, we have been eminently successful in reducing mortality and morbidity. The building of the Panama Canal would not have been possible without the elimination of mosquito transmission of malaria and also yellow fever -- and, for this, I am proud of my contribution.
So why, you might ask, is there so much malaria today? The answers are, in part, due to the plasticity of life: the drugs we use to treat patients with malaria are no longer effective because the parasites have modified themselves to become resistant to them. So, these infected individuals serve to infect mosquitoes. And, killing mosquitoes has become more difficult because they have become insecticide resistant. But, the limits to eradication are not only biological, they are also economic. Drugs against malaria parasites and mosquitoes cost money for development and deployment so that, in poorer countries, these monies are not available and it is the impoverished tropical countries where malaria remains a major killer. And, we must be ever vigilant, for from these foci, the disease may spread to other parts of the world; and, malaria poses problems, both for tourists and in the deployment of the military. Eradication is nowhere in sight.
(And now, in a dreamy fashion, he looks away and begins to talk as if to himself.)
Shakespeare, the greatest writer in the English language, knew that to have malaria was a fatal curse and he gave voice to this in Caliban's words; you know I, too, am a writer, though not so well-regarded as Shakespeare. But, is it merely a coincidence that we both recognized the importance of malaria?
Perhaps . . . (He leaves)